After surgery, chemotherapy, radiation, and reconstruction, for many HER2-positive breast cancer survivors, our next mission, should we choose to accept it, is to commit to a year of targeted immunotherapy, called Nerlynx. When I accepted the challenge, I decided to document my year on Nerlynx (neratinib) in hopes of helping fellow survivors trying to decide if they, too, should devote a year to this relatively new immunotherapy.



Who Should Consider Nerlynx
About 14% of all breast cancers today contain a protein identified as HER2+, and some cancer types can be like mine, “Triple Positive,” meaning Progesterone, Estrogen, and HER2+ fueled the cancer.
Typically, treatment includes surgery, chemotherapy, trastuzumab-based infusions (Herceptin), and radiation, followed by aromatase inhibitors to decrease the chance of recurrence. Additionally, in 2017 the FDA approved a drug, Nerlynx, which may also decrease recurrence by lowering the percentage of HER2+ cancer cells from binding in a woman’s body.
Nerlynx Research Statistics
In the ExteNET trial of 2840 patients, results showed invasive disease-free survival (iDFS) of 94.2% compared to iDFS of 91.9 in the placebo group. The five-year survival for Neratinib (Nerlynx) patients was 90.2 versus placebo (87.7%).
Patients with No PCR
More specifically, in the group of patients with no pathologic complete response (PCR) after chemotherapy (before surgery), the eight-year overall survival was 91.3% compared to 82.2%, making the drug a 9.1% benefit.
Patients with PCR
In patients with a pathologic complete response (PCR), the eight year overall survival was 93.3% with Neratinib compared with 73.7% with placebo, reflecting a 19.6% absolute benefit.
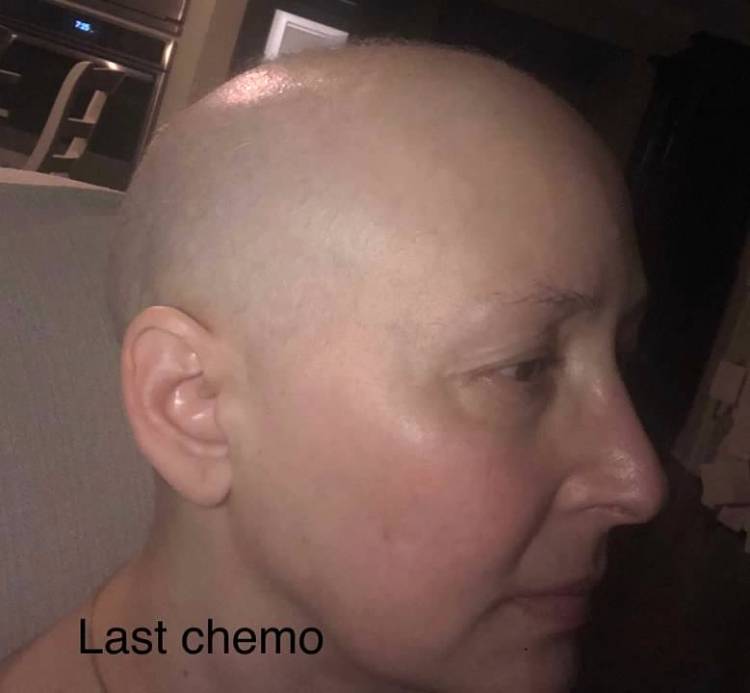
Committed to all I could to do to stay healthy, I pledged to take Nerlynx for a year. After all, after six hard chemotherapy treatments, 17 Herceptin infusions, radiation, and two major surgeries, I thought, “How difficult can six little pills be?”

The Wild Card: Nerlynx + IBS
No two breast cancer journeys are exactly alike, and I found the experience of taking Nerlynx to be no different. For instance, a friend of mine who also took Nerlynx warned me that the drug was not for the faint-hearted and that it took her body three months to adjust to the medication. After researching the side effects expected the first three months, diarrhea (possibly severe), nausea, abdominal pain, and fatigue, I still decided to take Nerlynx, not realizing that the side effects would remain a full year for me due to my past history of IBS.
Your Mission Should You Choose to Accept It
The Nerlynx biopharmaceutical company, Puma Biotechnology, advises patients to begin taking three tablets daily for a week, adding one extra tablet each week until reaching six tablets in three weeks, the dosage documented in their research. They say to take the medication with food, preferably in the morning, and to avoid grapefruit, antacids, alcohol, and multi-vitamins, especially calcium, for at least six hours after taking the medication since these items can make Nerlynx less effective. Puma Biotechnology’s researchers advise oncologists to prescribe Lomotil (because it is stronger than Imodium) to help patients manage the diarrhea while their bodies adjust to the medication. The representatives make it clear that taking Nerlynx is a personal decision to be made only after consulting one’s oncologist. However, they stand by their research claim that successful participants who took between three and six pills, six being their recommended dose, had a higher chance of survival versus those in placebo groups.
I’d like to point out that the dosage medication does not take into consideration the patient’s weight like other prescribed medications. Therefore, the same suggested dosage, six pills, is advised for a person weighing 125 lbs. as it is for a person weighing 225 lbs. I have shared this concern with Puma Biotechnology and hope they will consider tailoring the medication for each patient like most cancer-fighting drugs. I also asked them to consider studying patients with a history of IBS since I believe it plays a strong role in how the drug affects patients’ experiences. Puma Biotechnology currently has no research on patients with a history of IBS, so I hope this blog provides some incite for fellow survivors.
Aware of these guidelines, I first began Nerlynx in June, a month after ending Herceptin infusions. However, I was so sick with constant diarrhea that I stopped taking the drug after four days. I began it again in July, lasting about seven days on Nerlynx that time. I had been diagnosed with IBS (Irritable Bowel Syndrome) twenty years earlier but had not had an episode in over fifteen years. Unfortunately, I believe the medication, coupled with a tendency towards GI issues, caused the severe side effects of Nerlynx to be worse for me as opposed to someone with no prior history of IBS.
Third Time Is the Charm
In August, I decided time was running out since Nerlynx claims to be most effective taken within six months after completing Herceptin infusions, so I vowed to begin again and to commit to a year on the drug. I began Nerlynx on August 17, dealing with the usual diarrhea as before, but as I continued escalating the medication each week as advised by the drug’s representatives, the diarrhea got severe, and I burst a blood vessel in my bowel. As a result, I lost a lot of blood and had to take a steroid for a few weeks following the incident. I also added Budesonide, a different steroid typically used for Crohn’s disease, to my regimen of Lomotil and Imodium. On my third week, I visited the oncologist and was concerned that I had lost ten pounds and my red blood cell count was low due to the blood loss. Taking my oncologist’s advice, I reduced the medication to three tablets until my body could adapt to that dosage, which took three weeks. It took me from August until Thanksgiving to reach six tablets, and I highly suggest anyone with a history of IBS or Crohn’s disease ignore the manufacture’s general protocol of increasing a pill a week and, instead, increase the dosage whenever your body adapts to the medication, meaning whenever the diarrhea is controlled enough that you can maintain normal everyday activities.
To Each Her Own
People mean well, but when someone is diagnosed with cancer there is a lot of unsolicited advice, especially in regards to food. I’ve had well-meaning people suggest I avoid all sugar, gluten, preservatives, and tap water. Someone even urged me buy my own sauna if I wanted to beat cancer. Although people mean well, everyone’s cancer is different. For instance, mine is fueled by too much Estrogen, Progesterone, and HER2 protein in my body, so it is more complicated than simply going gluten free or vegan. I am told that there are a host of environmental factors most likely causing cancer today and that they could include everything from the ingredients in our toothpaste to the lotion on our skin; it is overwhelming and one can only do so much. Therefore, in order to survive a year of Nerlynx , I had to smile and ignore all the well-intended advice of others, especially regarding food, and eat what my body could digest: carbs, carbs, and more carbs, regardless of gluten or other preservatives. I began my day with bread and made sure I had bread with every meal to counter the impending diarrhea that came with eating. I followed the BRAT regimen closely (bananas, rice, applesauce, and toast) and avoided my triggers, which were caffeine, dairy, citrus, spicy foods, fried foods, alcohol, and desserts. From journaling my foods each day, I quickly discovered that the healthiest foods, such as salads, fruits, and fish, made the side effects worse, so I filled up on bread and crackers, bland foods to keep diarrhea down. Even with a constant carb intake, I was still losing weight because, although the side effects became manageable, they never ceased altogether for me when I was on the manufacturer’s recommended dosage. At Thanksgiving, when my plate consisted of a little turkey and a lot of rolls, a family member teased me, “What a diet. Eat bread. Still lose weight.” Unfortunately, there was truth to it. I was surviving on toast, crackers, and water for most of the year.
Dangers of Nerlynx
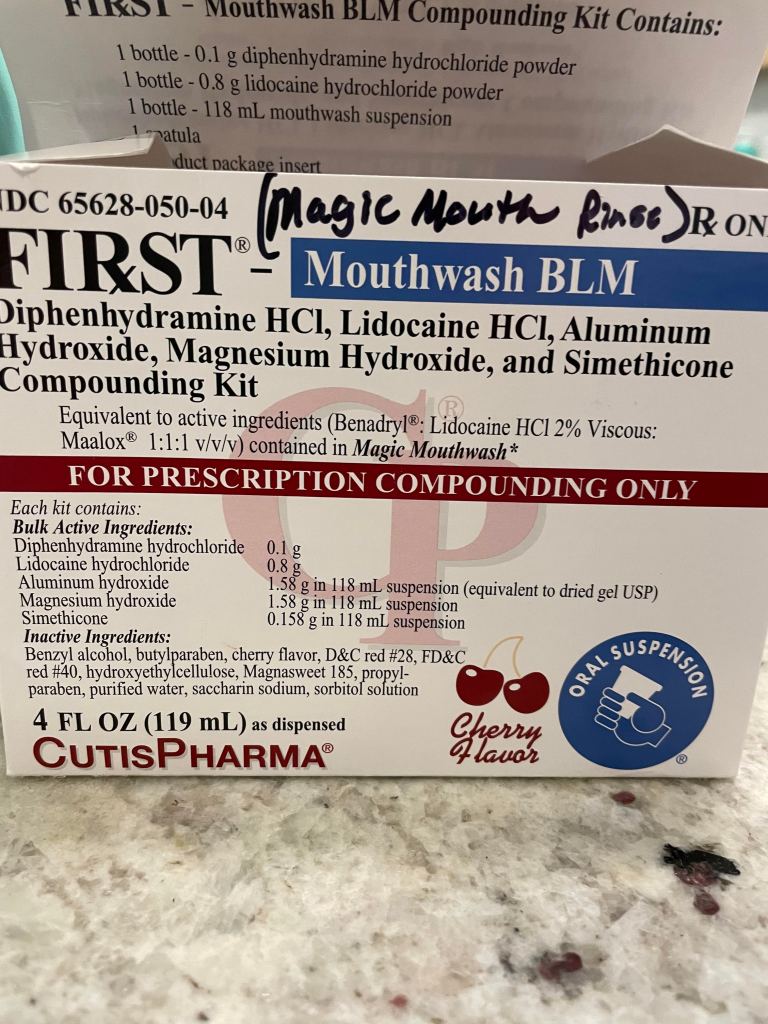
In addition to monitoring foods, the Nerlynx patient needs regular lab reports since the drug can affect liver function, so my oncologist monitored my labs carefully. Thankfully, my liver numbers never changed so drastically that I needed to stop the drug. Nevertheless, excessive diarrhea can decrease Potassium, a mineral needed for healthy heart function, so when a lab report indicated low Potassium, my doctor added a Potassium supplement to my regimen. I had been prescribed a Potassium supplement during chemotherapy, so I knew how hard the supplement was to ingest. The first time I tried swallowing the tablet, I almost choked because they are huge tablets. Next, I asked for the liquid form of Potassium, but its taste made me extremely nauseous. Finally, a pharmacist suggested I try the capsule form and break it open, mixing it with apple sauce. It has been the best solution for me, and I hope it helps someone else struggling to take Potassium, which is commonly prescribed for cancer patients.

The Mystery Rash
Thinking I had experienced all the Nerlynx symptoms, I was surprised one morning when I woke up to a rash over my nose and across my face. It looked like red fluid-filled bumps that I couldn’t identify. After a week I visited a dermatologist who tested the rash for MRSA, Staph, and Strep. Luckily, all tests were negative, but it was still a mystery to me and the dermatologist. It itched and burned a little at the same time. When I reached out to the CVS Specialty Pharmacy, the company who supplied me with Nerlynx and monitored me regularly, the pharmacist said he had heard complaints of rashes in 2/10 cases. He advised washing with Hibiclens (found at any drugstore) and using Eucrisa or over-the-counter Hydrocortisone cream. He also suggested adding a probiotic to my diet but at the end of the day so it did not interfere with the Nerlynx. In the end the rash spread to my eyelids, so it got frightening, but it never really hurt and was not contagious to family members, so I continued with the Nerlynx. Unfortunately, the rash came and went for the remainder of the year. The pharmacist also warned me that sun could cause the rash to flare up, and he was correct. My first beach trip in three years ended with a rash on both arms and legs, but at least I knew it was temporary.


Dry Eye Syndrome and Nerlynx
Like so many Americans, I was diagnosed with Blepharitis about ten years ago. Basically, I have clogged oil glands in the eyes causing dry eyes. Since the Blepharitis diagnosis, I have taken high doses of Fish Oil, prescription eye drops, and used moist eye compresses to decrease dry eye symptoms. With Nerlynx, a typical day meant taking four Lomotil pills to control diarrhea, which is equivalent to eight Imodium pills. Unfortunately, controlling diarrhea also meant drying out my oil glands as well. To make matters worse, the heat compresses suggested to open oil glands made the rash worsen on my eyelids. At one point I developed a chalazion, blocked oil gland, and had to have an eye specialist complete an in-office procedure to unclog it, which left me with a painful black eye for a week. It was a vicious cycle, but I reminded myself frequently that it was only for a year, and I tried to focus on the step before me and not the staircase.
Walking a Tightrope
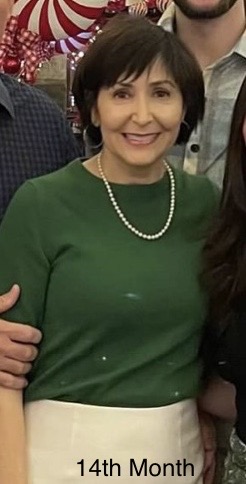
By May, I had lost fifteen pounds and felt exhausted all the time. Unfortunately, the side effects of Nerlynx never slowed for me even eight months into taking the drug. My days consisted of decreased appetite and several bouts of severe diarrhea, sometimes with very little warning, causing me to wash my soiled clothes all day long. I was grateful that I could work from home and rarely left the house for fear of the consequences. For the first time in my life I dreamed of salads and fruit instead of desserts or breads. Agonizing over how to maintain my committed year yet still have some quality of life, I finally decided to decrease the medication from six pills a day to four. After all, I only had three months left. Within a week I was able to have a little fruit or a cooked vegetable, and within a month I could eat a whole salad or a portion of fruit. By July with only a month to go, I could treat myself to a frozen yogurt bar in the evening when most of the four pills was out of my system. Alcohol, unfortunately, never got easy, but I made sure it was only on special occasions. For the remainder of the time, I stayed on the Budesonide since it contained an anti-diarrhea ingredient and often still took Lomotil, but I could eat more foods and leave the house with more confidence. With four pills, I finally found balance on Nerlynx.

Doing It All Over Again?
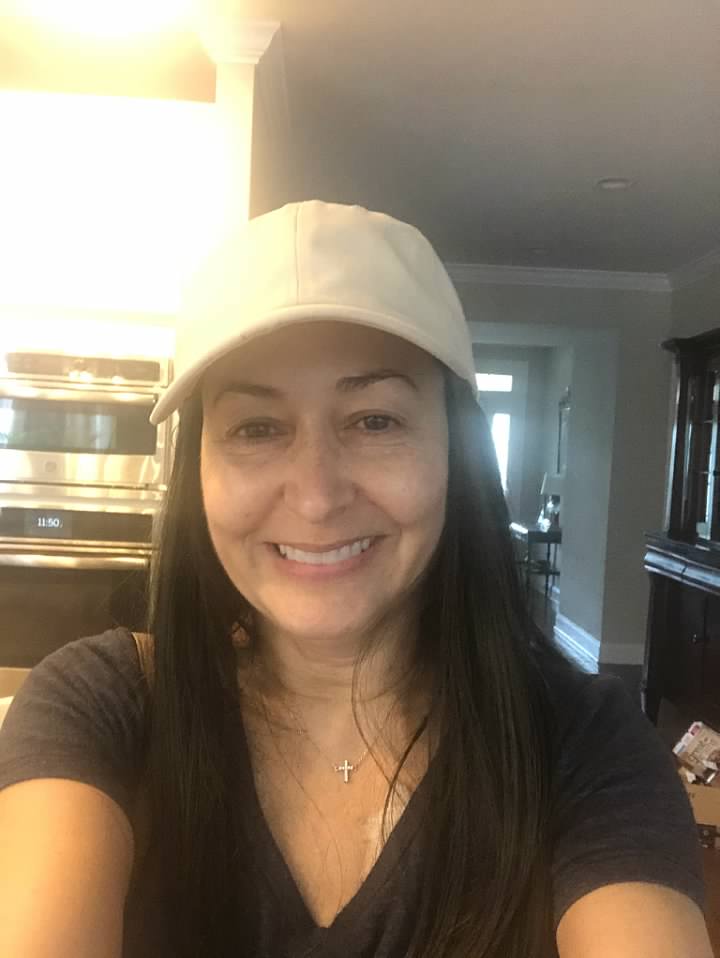
Some survivors finish chemo and never take Nerlynx at all. At times I wish I could be more like that but I am built differently. I am a person who must do everything offered to me so that I don’t have to live wondering if I could have done more to remain healthy. While Neralynx was a beast for me, it is not the case for everyone. My recent body scan showed that I have been cancer free for two years, which I am celebrating. Three years will be a huge milestone for me, and five years is considered “graduated” in the medical community. I have concluded that I would do it all over again but instead of taking the full dose, I would remain on four pills in order to have a better quality of life. Although Nerlynx was a difficult mission, I am at peace having completed the recommended 365 days on the medication. If I have gained any wisdom from going through cancer, it is that peace of mind is a beautiful place to dwell.
“You were given this life because you are strong enough to live it “
Ain Eineziz
This blog is dedicated to Joanna Rose, my fellow cancer researcher, survivor, prayer warrior, and dear friend.